Before surgery
- I listen to the reasoning for gender transition or wanting to have a more feminine voice.
-
I record the following:
-
Reading of a standardized passage (Man’s First Boat), documenting what I call the Comfortable speaking pitch.
- I typically record this passage at the attempted best female voice.
- I record the passsage again at the most relaxed, and typically male voice.
- It doesn't hurt to have recorded some spontaneous conversational speech in the recording as well.
- Maximum phonation time (at the comfortable speaking pitch)
-
Vocal pitch range
- Record the lowest note that can be produced
- Record the highest note that can be produced
- Maximum volume - essentially a yell
-
Vegetative sounds are recorded.
- A cough
- A Throat clearing
-
Minimum volume
- I record soft singing of "Happy Birthday to You" at low, medium and high pitch.
-
Reading of a standardized passage (Man’s First Boat), documenting what I call the Comfortable speaking pitch.
- The vocal cords are then visualized and video recorded with flexible laryngoscopy including stroboscopy at a variety of pitches and volumes.
At Surgery
Location: All surgeries have been performed in a Medicare certified, outpatient surgical center. The procedure is typically two hours long.
Anesthesia: The procedure is performed under general endotracheal anesthesia using a 6-0 endotracheal tube. (It is not a particularly painful surgery and I performed the first one under local anesthesia. However, I did not like that the patient was trying to talk while I was trying to suture the vocal cords. I worried that I was going to tear them.)
Antibiotics: I use two perioperative antibiotics at the time of surgery:
- clindamycin - 600 mg
- cefotaxime or levofloxacin.
- I also irrigate with normal saline containing 100,000 units per liter of bacitracin prior to incision closure.
- I give 7 days of post-operative oral therapy with either cefuroxime or levofloxacin.
Steroids: 10 mg of dexamethasone are given intravenously at the beginning of surgery. Oral prednisone or methylprednisolone are given in selected cases if significant swelling develops postoperatively.
Technique:
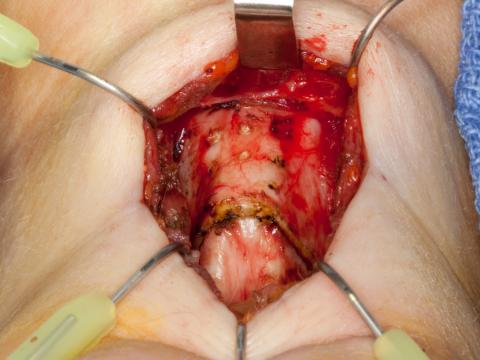
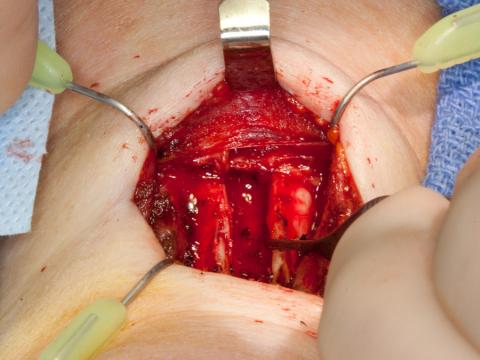
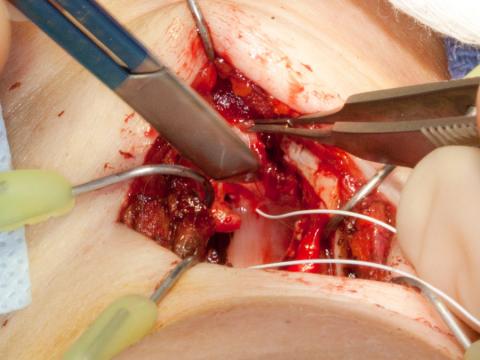
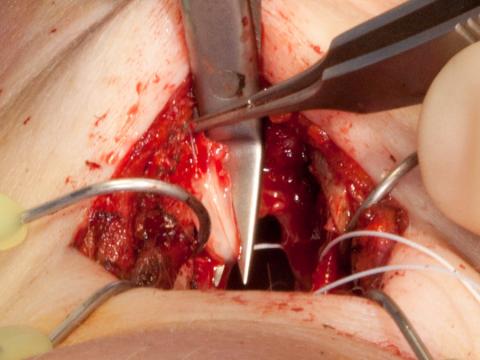
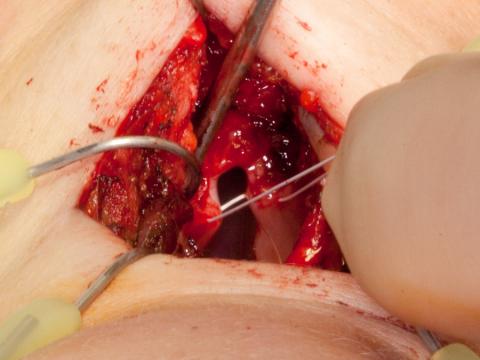
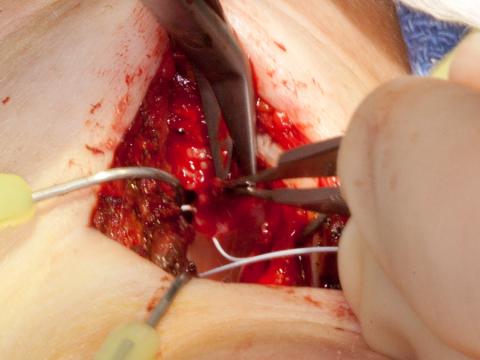
(All photos are taken from the perspective of the anesthetist at the head of the table. So you are looking over the chin at the neck.)
An approximately 5 cm incision is placed in or parallel to a skin crease directly in the midline
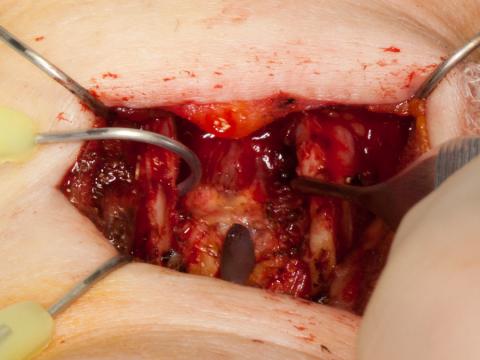
Flaps developed at a level beneath the platysma.
Strap muscles are visible.
The strap muscles are separated in the midline exposing anatomy from the hyoid bone to the upper cricothyroid membrane (marked here with a bovie cautery cut). This exposes a good view of the thyroid cartilage or Adam's apple.
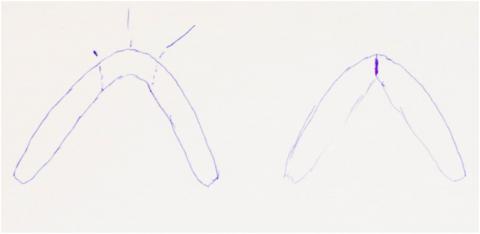
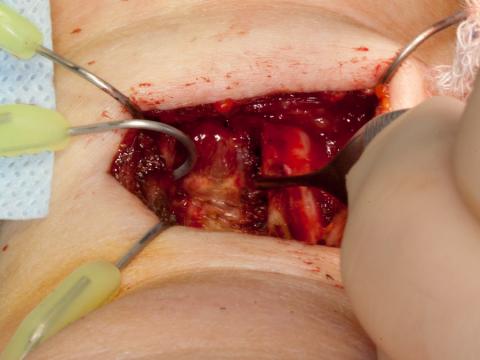
The midline is marked with a Bovie cautery and secondary marks are placed 5 to 7 mm lateral to the midline on each side. I have also marked the upper incision to remove the upper alae of the thyroid cartilage.
If a thyrohyoid elevation is planned, the upper portions of the thyroid cartilage aare removed at this point (or later after division of the thyroid cartilage in the midline).
The thyroid cartilage is divided vertically with an oscillating saw about 3 to 7 millimeters on either side of midline with the saw kerf removing about one additional millimeter of cartilage. The goal is to narrow the internal aperture of the laryngeal glottis by collapsing the thyroid alae medially.
Beveling the cuts: Cuts placed at a 90 angle to the cartilage allow only the inner thyroid lamina to approximate. The inner lamina is more contoured than the outer lamina with an internal bulge inferior to the vocal cords. A 90-degree cut thus prevents an airtight closure unless these contours are then removed with a cutting burr. By comparison direct saggital cuts allow only the outer lamina to approximate when the alae are collapsed back into the midline. Consequently, I attempt to bevel the cuts between these two planes to allow complete, airtight closure of the new anterior larynx in the midline.
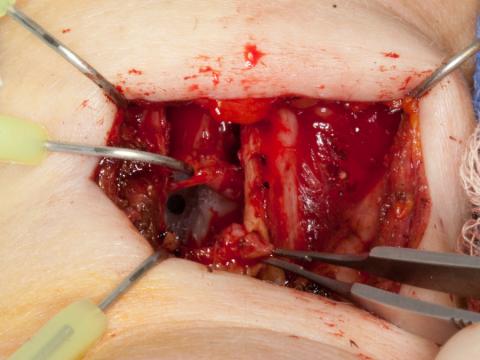
With electrocautery, the strip of anterior thyroid cartilage is elevated away from the soft tissue and removed. This removal of the vertical anterior thyroid cartilage segment will both narrow the internal laryngeal aperture and very effectively remove the Adam’s Apple contour (more completely than a “tracheal shave”). The airway is not typically entered, although if it is, penetration usually occurs in the thinnest area, which is just superior to the anterior commissure.
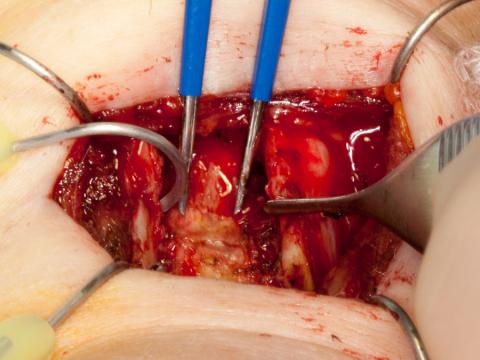
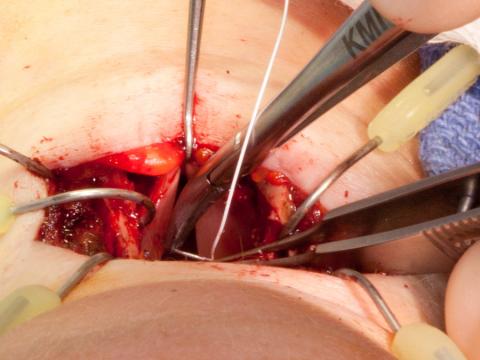
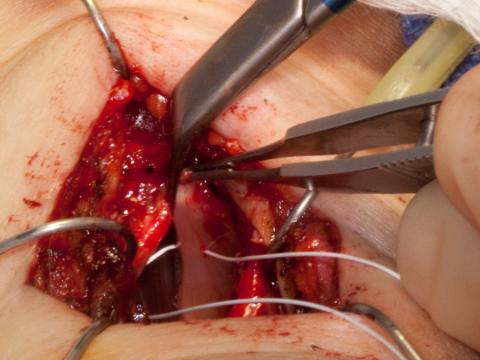
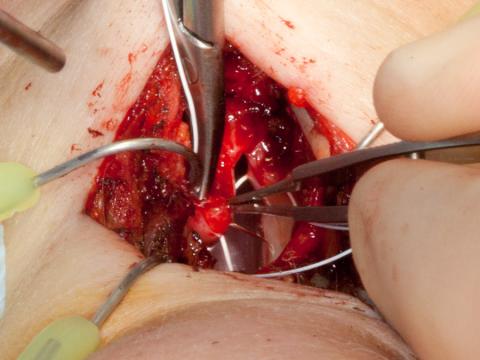
The thyroid alae may be retracted laterally for a better view of the internal glottis.
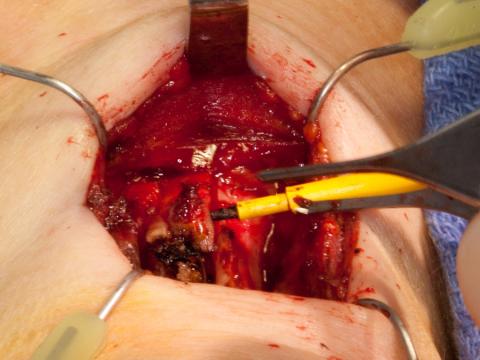
The vocal cord anterior ligaments are identified (blue electrocautery tips point to the ligaments).
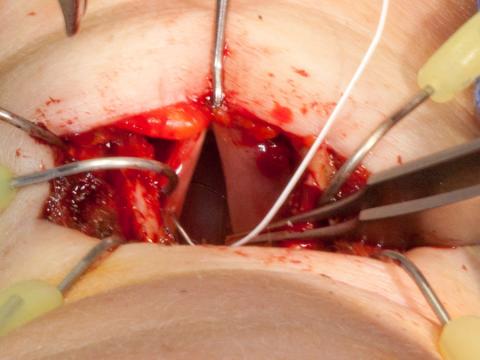
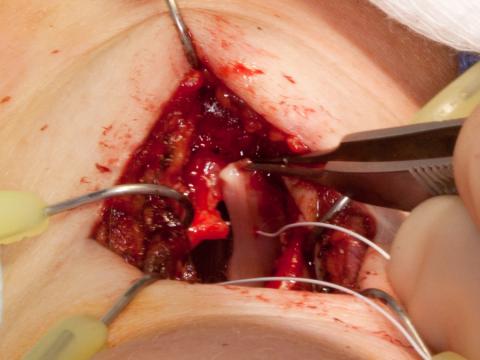
The airway is incised just superior to the anterior commissure.
Extend this midline incision superiorly through the anterior commissure of the false vocal cords for a view of the endotracheal tube and the true vocal cords from above.
I remove approximately the anterior 25% of each false vocal cord, including the saccule. This reduces the diameter of the supraglottis after surgery. During surgery, this also provides an improved view of the true vocal cords and more space to manipulate needles within the larynx.
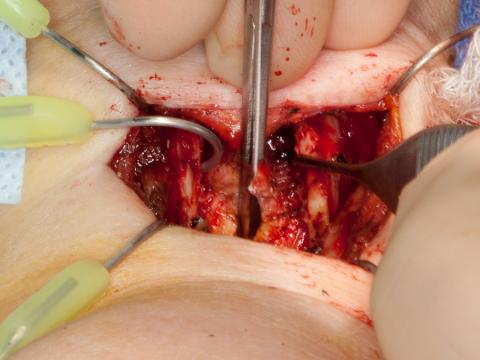
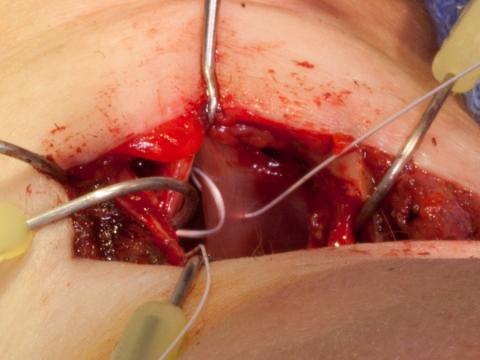
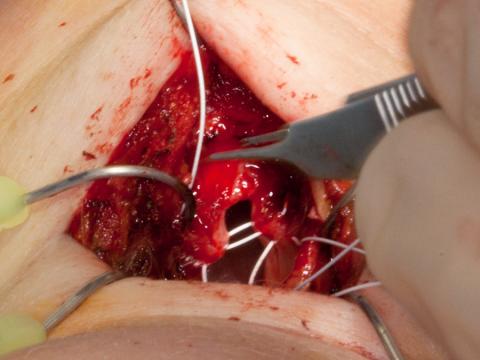
I prefer to maintain the anterior glottic ligament intact so that I can pull symmetrically on the vocal cords with a hook. I assess how much of the anterior vocal cord needs to be removed in order to collapse the thyroid alae back into the midline while maintaining tension on the vocal cords.
As I stretch them, I use one half of a double-ended 4-0 polytetrafluroethylene (Gore-Tex) suture to mark the perceived 50% location along the membranous vocal cords as measured from the anterior commissure to the tip of the vocal process. I try to include the vocal ligament in this suture to maintain not only a symmetric length to the neo-vocal cords, but also to maintain the vibratory margins vertical symmetry. My anticipated goal is to remove about 40 – 50% of the anterior membranous vocal cord. With removal of the anterior thyroid cartilage, the anterior-posterior dimension of the larynx will be smaller, so more membranous vocal cord must be removed to raise pitch than in a straight thyrotomy where only a small amount of vocal cord resection will raise pitch to some degree.
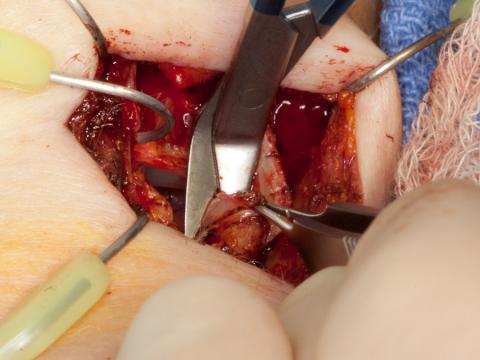
I divide the anterior commissure, attempting to minimize the length of the incision inferior to the vocal ligaments. My goal is to keep the inferior extent of the excision beneath the lower boundary of the thyroid cartilage. If the subglottic incision continues beyond the inferior edge of the thyroid cartilage into the cricothyroid membrane, it is more difficult to obtain an airtight closure.
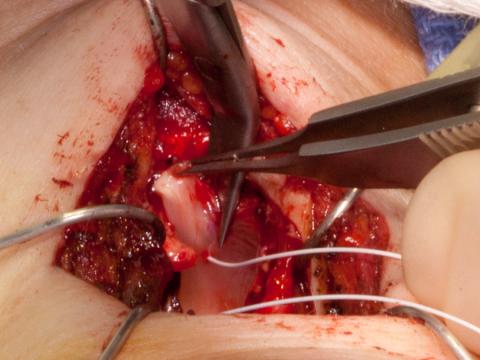
While tensioning each cord by grasping the anterior vocal ligament, right-angled scissors cut through the membranous cord.
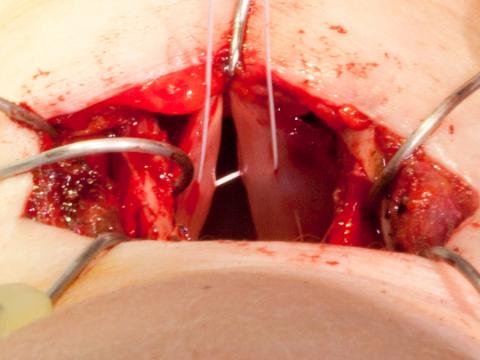
The mucosal cuts are beveled from lateral to medial. At the lateral aspect the cut is at the edge of the inner lamina of the thyroid cartilage.
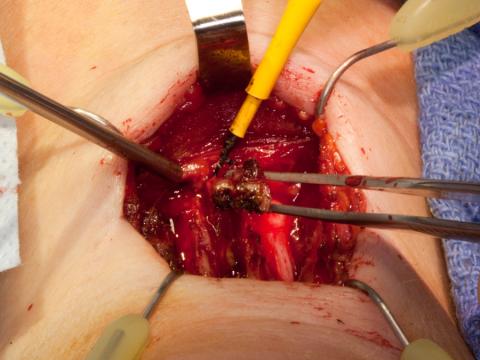
Medially the cut exits the cord just anterior to the marking suture. The mucosa, vocal ligament and the thyroarytenoid muscle are included in the removal.
An identical amount is removed from the opposite vocal cord.
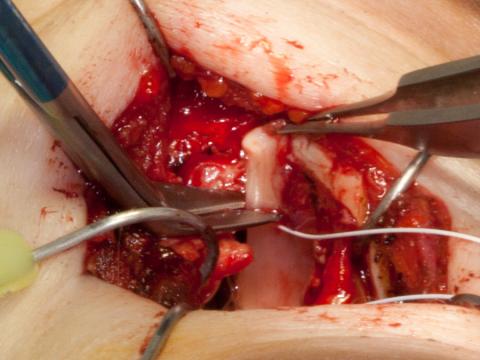
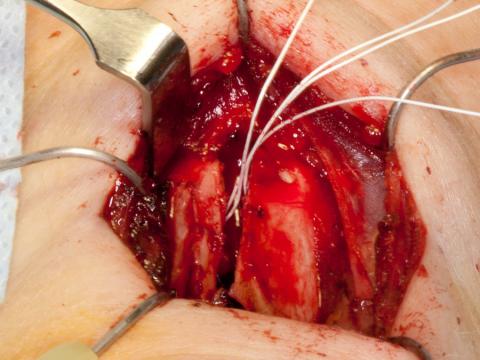
The cut edges of the thyroid cartilage are laid back together into their future position to check first for accurate coaptation. The cartilage is typically thicker just inferior to the attachment of the vocal cords. If tight closure is precluded by an inappropriate saw angle or because of any variation of thickness in the cartilage, these are removed or adjusted with a burr at this time.
Secondly, the vocal cords are stretched as the thyroid lamina are brought back together to verify they are not too long to be placed under tension when secured against the inner thyroid lamina. If they will not be under adequate tension, then more vocal cord can be removed.
At times, the issue seems to be too much tissue bulk. I then grasp the central thyroarytenoid muscle, place it on a stretch and remove or debulk some additional muscle, typically nearly the anterior half of the thyroarytenoid muscle.
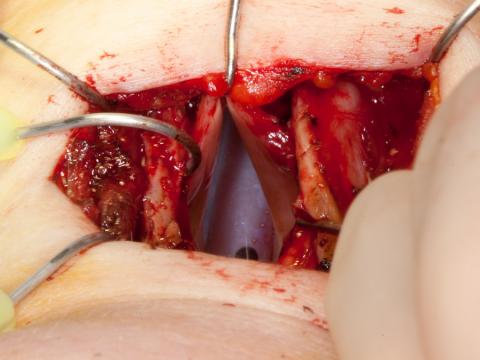
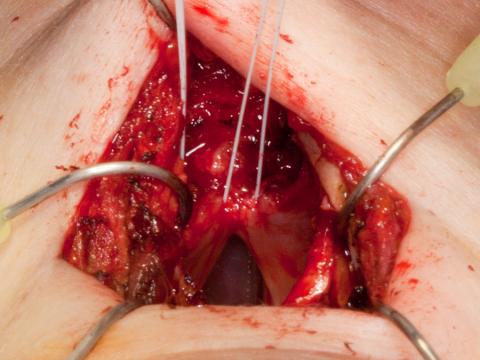
Anterior commissure reconstruction: Using a Gore-Tex suture, I place a horizontal mattress suture into the vocal cords. The needle enters the left thyroarytenoid muscle, passes through the vocal ligament (which feels slightly dense) and includes about 1 mm of medial margin vocal cord epithelium. I attempt to exit at what I perceive to be the upper vibratory lip of the membranous vocal cord.
This passes into the opposite cord in a similar location beginning with the vocal cord epithelium and passes out through the thyroarytenoid muscle. I re-pass the needle back following a path about 1 mm inferior at what I perceive will be the new inferior vibratory lip of the membranous vocal cord. Both ends of this first suture exit the left thyroarytenoid muscle.
If I pull on the marking suture, I can visualize the neo-vocal cords.
I remove the Gore-Tex marking suture, reusing it, passing it in opposition using a similar pathway beginning with the right thyroarytenoid muscle. At the conclusion, both ends of one suture exit the left vocal cord and both ends of the other suture exit the right vocal cord. Pulling on these brings the new anterior commissure together.
One reason that I use Gore-Tex is that when the thyroid alae are brought back together, the slipperiness of the Gore-Tex allows it to slide between the cartilage.
Please download the pdf for surgical technical information on feminization laryngoplasty and thyrohyoid elevation.